Dr. Megan Beers Wood, of Johns Hopkins School of Medicine, published the results of her most recent work on pain hyperacusis in February 2024 and her full paper is found here. This work was funding in part by Hyperacusis Research through our partner, Hearing Health Foundation (HHF), with their Emerging Research Grants program. Dr. Wood has kindly provided a summary of her detailed paper, which appears here. Thanks to HHF which originally published this summary here.
By Megan Beers Wood, Ph.D.
The mammalian cochlea has a problem. The evolution of sensitive hearing over a wide frequency range has produced a biomechanically complex sense organ, but one vulnerable to irreparable damage.
In addition to causing hearing loss, damage to the inner ear (cochlea) can also lead to conditions like hyperacusis, where everyday sound levels become unbearably loud and painful.
Adding insult to injury, the associated pathology of hyperacusis can undermine quality of life as much or even more than partial hearing loss. Research continues to identify the underlying pathological mechanisms of hyperacusis.
It has been proposed that pain hyperacusis (noxacusis) may be transmitted to the brain by sparse, unmyelinated nerve fibers called type II cochlear afferents. These fibers share similarities with pain-sensing nerves in the rest of the body, such as in the skin.
One hallmark of skin pain is the release of adenosine triphosphate (ATP), a cellular energy molecule, causing a rise in calcium within epithelial cells. Around a point of damage, this produces a “calcium wave” spreading from the site of damage.
These calcium waves contribute to activation of pain-sensing neurons in the skin that transmit the pain signal to the brain. Calcium waves also occur in the inner ear.
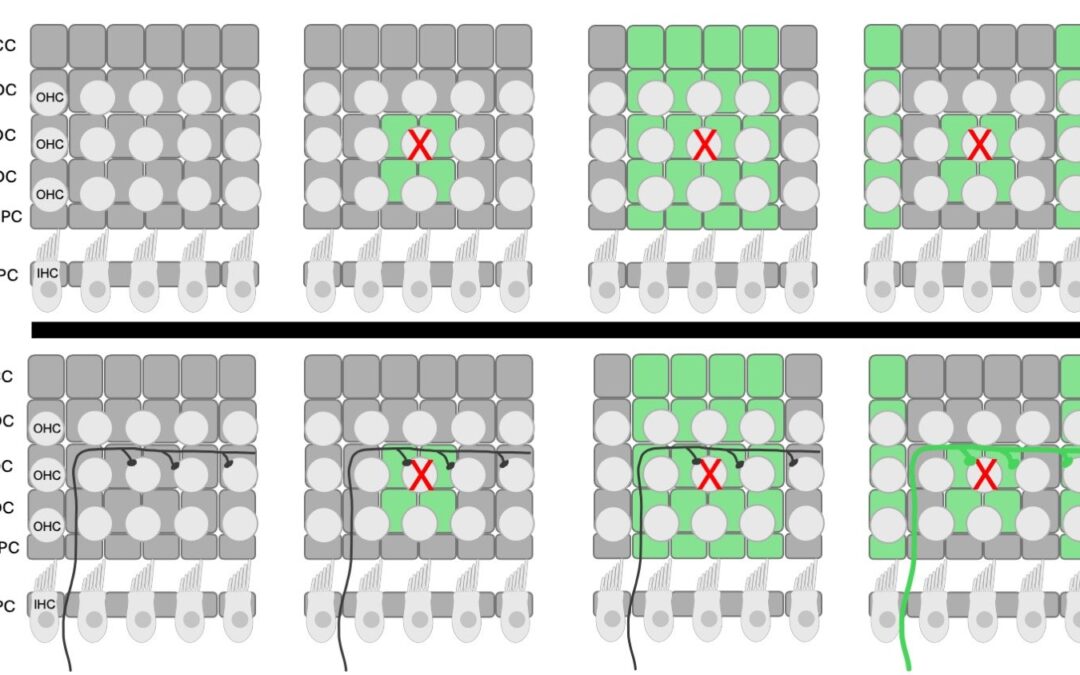
The diagram is a top-down view of the organ of Corti with three rows of outer hair cells (OHC) (represented by gray circles) and a single row of inner hair cells (IHC). The dark gray rectangles represent the supporting cells underneath the hair cell layer. From top to bottom, there is one row of Claudius cells (CC), three rows of Deiters’ cells (DC) and two rows of pillar cells (OPC and IPC). The outer and inner pillar cells are separated by the tunnel of Corti. The top row is a schematic showing how fluorescence (green cells) propagates from the site of damage (OHC marked with red X). The arrow indicates time. The bottom row is the same schematic with a single type II afferent added to show the timing of type II activation relative to the fluorescent wave in the epithelial cells. After noise exposure, the type II afferent calcium-associated fluorescence occurs after the initial epithelial cell wave. Credit: Wood, Megan Beers; Nowak, Nate; Fuchs, Paul Albert/Frontiers in Neurology
In our previous paper in eNeuro in 2021, we showed that an increase in calcium occurred in both epithelial cells and type II afferents after focal damage caused by a laser.
In our new mini-review published in the journal Frontiers in Neurology in February 2024, we focus on cochlear epithelial cells to highlight another tool for studying damage-evoked calcium waves.
There is an increase in fluorescence (a glowing signal) that is visible without calcium-sensitive dyes or genetically encoded calcium indicators.
This signal is thought to result from an increase in the fluorescent molecule NADH. When the calcium wave triggered by cochlear damage enters the mitochondria of cells, it causes an increase in the production of fluorescent NADH from its non-fluorescent form NAD.
The resulting waves of increased fluorescence propagate through tissues similarly (speed and dissipation with distance) to the calcium waves described previously in the cochlea and skin using genetically encoded calcium indicators. Importantly, these waves can be studied in any tissue since no calcium indicators are required.
Of relevance to hyperacusis, prior noise-induced hearing loss leads to the generation of prolonged and repetitive activity in type II neurons and surrounding tissues. This aberrant signaling may be the basis for the sensitivity to everyday sounds seen in hyperacusis. We will continue to explore the activity of epithelial cells and type II cochlear afferent fibers as the cellular basis for pain hyperacusis.
Thank you for continuing the research on Hyperacusis Pain. I enjoyed reading about the research and results. My son is going on 10 years being affected by this hyperacusis pain.
As someone who has endured severe pain Hyperacusis for most of my entire adult life, I remain encouraged by the continuing research by Dr. Wood into the role these type II nerve fibers play in sensing ear pain and transmitting this to the brain. My desperate search for help over 12 years ago, led me to Bryan Pollard. We communicated numerous times after that via phone and email, and he was the first person that I had talked with that truly understood and cared. He became a source of information and understanding, and most of all, a friend. He would most certainly be so very optimistic and pleased with results like this from the ongoing research into causes of pain Hyperacusis. Thank you, Dr Wood.
This post is extremely radiant. I really like this post. It is outstanding compared to other posts I’ve read in quite a while. Much obliged for this better-than-average post. I truly value it!
Comment * thank you very much for dealing with hyperacusis pain. It gives me and millions of people hope for healing. I hope you can do it as soon as possible. Fingers crossed.
And what practical solutions coming out of that founding?
That’s what I’d like to know
Thank you to everyone involved with this research! I plan to send this article to family and friends when they want to learn more about Hyperacusis. The more we can understand it, the closer we can get to finding treatment or a cure.
Thank you so much for publishing this summary of the Megan Beers Wood paper!
It seems to go along with what I know of my own situation. In 2019 an occupational therapist who has helped a number of hyperacusis patients tested me and my (horrible) hyperacusis. She found that signals from the left ear and from the right ear are reaching the brain at different moments. She believes this malfunction is the cause of my own hyperacusis. Most importantly though, she found therapy to help me. Not cure, but help.